With PDABs becoming increasingly popular throughout the country, HealthHIV is advocating for the crucial needs of patients amid rapid policy change, and critical conversations happening on this subject.
HealthHIV seeks to:
- Protect access to lifesaving medications
- Push forward and uplift initiatives to ensure equitable medication uptake
- Preserve critical public health efforts
- Promote the patient voice in all healthcare policy discussions
What is a Prescription Drug Affordability Board?
A Prescription Drug Affordability Board (PDAB) is an oversight entity established by states to evaluate and manage the costs of prescription drugs. Its primary objective is to ensure drug affordability for consumers while balancing state healthcare budgets. PDABs conduct “affordability reviews” of drug prices and spending, and develop strategies to control costs.
A key tool in their arsenal is the implementation of Upper Payment Limits (UPLs), which set maximum price caps that state programs will pay for certain medications.
What’s at stake for patients?
- Affordability, from a patient perspective, means access to essential medications and treatments without facing financial hardship, ensuring equitable healthcare access and robust patient protections.
- Patients may face limited access to specific medications if manufacturers do not lower their prices to meet UPLs, potentially affecting their ability to obtain essential treatments.
What’s at stake for providers?
- For providers, it involves delivering quality care without being constrained by cost considerations.
- Providers may need to consider alternative medications for their patients based on UPLs and affordability, potentially altering treatment plans and impacting patient care.
What’s at stake for payers?
- Payers work to strike a balance between controlling expenses and safeguarding patients’ equitable access to necessary healthcare services.
- Payers must navigate changes in drug pricing strategies and formulary designs due to UPLs, potentially affecting which drugs are covered and how costs are shared with patients.
Latest Resources

Prescription Drug Affordability Boards (PDABs) and Upper Payment Limits (UPLs) Impact on Patients, Drug Pricing, and Innovation
This HealthHIV Advocacy paper explores the function of Prescription Drug Affordability Boards (PDABs) in managing prescription drug costs, considering perspectives of patients, providers, and payers to ensure equitable access to vital medications while controlling healthcare expenses.
Considerations and Implications of PDABs and Their Impact on 340Bs
Prescription Drug Affordability Boards (PDABs) are designed to help reduce the costs of prescription medications in 11 states where they currently exist (legislation pending in 13 more states).
PDAB: Balancing the Scale
The Role of PDABs in Drug Pricing and Healthcare Stakeholder Impacts

PDAB Action Steps for Patients
Patients looking to contribute to the conversation about drug affordability and Upper Payment Limits (UPLs) can start here.
PDAB Action Center
This info, along with our (coming soon!) Social Media Sample Posts, PDAB Letter Template, PDAB Policy Resources, and Submitted State Comments and Coalition Letters, offers a straightforward way to help inform your thoughts and concerns, share your experiences, and actively participate in shaping policies that directly impact patient care and access. We will be posting all of these documents and items to this Resource Center soon.

Action Steps for Patients
Patients looking to contribute to the conversation about drug affordability and Upper Payment Limits (UPLs) can start here. Click to download.
- With momentum provided by the 2022 Inflation Reduction Act, close to a dozen states have implemented—or are considering implementing—Prescription Drug Affordability Boards (PDABs) in order to tackle drug costs. Learn more here: https://healthhiv.org/pdab/
- Prescription Drug Affordability Boards (PDABs) introduce a new and complex dynamic in the ongoing efforts of public and private entities to negotiate drug prices and reimbursement rates. Read #HealthHIV’s latest advocacy paper on PDABs here: https://healthhiv.org/resource/prescription-drug-affordability-boards-pdabs-and-upper-payment-limits-upls-impact-on-patients-drug-pricing-and-innovation/
- Prescription Drug Affordability Boards (PDABs) must balance system-wide financial concerns with the actual impact on patients’ out-of-pocket costs. Explore #HealthHIV’s PDAB Resource Center to learn more about this: https://healthhiv.org/pdab/
- Overall, PDABs’ approach must balance broader—system-wide—financial concerns with the actual impact on patients’ out-of-pocket costs, but does not always do so.
- The evidence regarding the effectiveness of PDABs in reducing list prices or reimbursement rates is also still emerging, and it remains to be seen whether and how these reductions will actually translate into real-world direct savings to patients.
- Existing evidence does suggest, however, that the impact of PDABs on reducing patient out-of-pocket costs and enhancing access to medication remains complex, and varies from state-to-state.
- While PDABs are meant to analyze statewide drug pricing and recommend strategies to lower patient spending, their effectiveness largely depends on factors like the existence of cost-offsetting patient assistance programs, and better access to both real-world and claims data.
- PDABs must work with patients and stakeholders across various disease states and conditions—whether rare, orphan, or communicable—to serve the dual goals of both preserving and improving medication access, and containing costs.
- Only with these dual goals—and this broader context—as PDABs’ north star will the needs of patients truly be put first.
PDABs by State
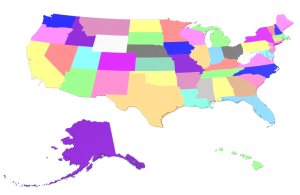 Learning from Other States: States like Minnesota may look to the experiences of others, such as Colorado, Oregon, and Maryland, to learn from their approaches, challenges, and successes. This can help tailor policies to address their healthcare systems’ and patient populations’ specific needs and circumstances.
Learning from Other States: States like Minnesota may look to the experiences of others, such as Colorado, Oregon, and Maryland, to learn from their approaches, challenges, and successes. This can help tailor policies to address their healthcare systems’ and patient populations’ specific needs and circumstances.
- Engagement and Transparency: All these states are showing varying levels of commitment to engaging with stakeholders, particularly patients, to ensure that the policies developed are reflective of community needs and real-world impacts.
- Legislative Progress and Challenges: Each state is at a different stage in their legislative process concerning drug affordability, with some like Illinois seeing stalled efforts and others like Vermont advancing significantly.
- Patient-Centric Focus: There’s a clear trend towards ensuring that any drug pricing or affordability measures consider the unique needs and circumstances of patients, aiming to prevent negative impacts on access to necessary treatments.
- Discussion Points: Similar to Oregon, discussions in Colorado also touched upon concerns related to fear and anxiety among patients regarding access to medications under the potential upper payment limit (UPL) settings.
- Patient and Public Engagement: Efforts are being made to engage more directly with patients and public stakeholders to better incorporate their inputs into the decision-making process.
- Expansion of UPL Process: The UPL process is being expanded with more opportunities for stakeholder input scheduled through December.
- Advisory Role Development: Plans to recruit advisors over the summer to help refine processes and perhaps include patient representatives directly in the advisory process.
- Legislative Status: Bills were introduced to establish a health care availability and access board to revise the costs of prescription drug products. However, these bills missed procedural deadlines, indicating no immediate activity expected.
- Future Prospects: There is a potential for rules suspension which could revive discussions closer to election times, but currently, no major movement is expected.
- Initial Review Approval: Maryland approved an initial review of certain drugs, with a focus on ensuring therapeutic alternatives are considered. They are particularly aware of the heterogeneity of diseases and the unique needs of patients.
- Stakeholder Engagement: The state is actively inviting feedback on why substituting therapeutic alternatives could be problematic, highlighting an openness to understanding patient-specific treatment needs.
- Issues Encountered: The PDAB in Oregon experienced unprofessional behavior and pressure, highlighted during a meeting where there was a notable “rant” by a board member. This incident reflects the board’s stress due to the lack of public engagement, as town hall meetings were poorly attended and had minimal patient input.
- Response to Public Input: Despite efforts to facilitate participation, such as providing translators, the PDAB seems up against significant challenges in obtaining meaningful public and patient input.
- Future Engagements: There are upcoming virtual meetings on the 8th and 14th that are crucial opportunities for further public and stakeholder engagement.
- Progress in Legislation: A bill in Vermont has made significant progress, passing through the Senate with an amendment requiring consideration of patient access in drug affordability reviews. It has proceeded through the necessary House Committees and is expected to reach a House vote soon.
- Focus on Patient Access: The amendment specifically aims to ensure that drug affordability reviews take into account the impact on patient access, reflecting a balanced approach to cost and care.
- Early Stages of Process: Washington is earlier in the process compared to other states. There’s a focus on involving patient organizations and caregivers in developing the process, surveys, and outreach strategies.
- Future Engagement Opportunities: The state plans to include patient representatives in advisory panels, signaling a commitment to including patient voices in decision-making processes related to drug pricing.
- Engagement Necessity: Both states highlight the necessity of engaging more effectively with the public and especially with patients to ensure that the PDAB processes are inclusive and reflect real-world impacts and concerns.
- Transparency and Education: There is a significant need for transparent processes and educational outreach to ensure that stakeholders, particularly patients, understand what UPLs entail and how they might affect access to necessary medications.
- Coalition Actions: The coalition plans to develop principles, draft coalition letters, and engage more robustly with state boards to ensure that patient voices are heard and integrated into the policy-making process.